Thanks to optical coherence tomography angiography (OCTA), optometrists are poised to advance their capabilities and role in caring for diabetic patients. OCTA is a non-invasive imaging technique that generates volumetric angiographic images without the use of an intravenous dye (fluorescein or indocyanine green) in a matter of seconds. Data produced by these images can detect microvascular changes in the retina of a diabetic patient up to two years before retinopathy can be detected via photography or ophthalmoscopy.
Here is how this technology, along with use of a clinical outcome registry, can transform and expand your diabetic eyecare services.
A New Way of Approaching Diabetic Patient Care
Historically, the scope of optometric practice expanded following authorization to use diagnostic and therapeutic drugs. Further expansion resulted after the American Optometric Association (AOA) successfully persuaded Medicare to recognize optometrists as physicians for reimbursement. With the use of OCTA, optometrists are now at the brink of a new opportunity to measure and track detailed microvascular changes in the retina. These findings include: the size of the foveal avascular zone (FAZ), areas of abnormal flow in the outer retina and choroid, vessel density of the superficial vascular complex, deep vascular complex and radial peripapillary capillaries.
In the past, diabetic patients who were shown photographs of their retina to demonstrate diabetic retinopathy often became more conscientious about controlling their diabetes. However, using OCTA data, microvascular changes can be demonstrated to the patient well before visible retinopathy occurs. This is an opportunity to demonstrate physical changes and risk of retinal complications to encourage better control of HbA1C much earlier in the process. Optometrists can now demonstrate to patients these measurable abnormal microvascular trends over time.
Going one step further, combining these data with a clinical outcome’s registry can provide patients with clinical outcomes from a group of similar patients to project their current risk of more advanced complications based on their HbA1C level. Discussing, practicing and prescribing in this manner employs data analytics and is truly based on objective clinical results from a comparable population of patients.
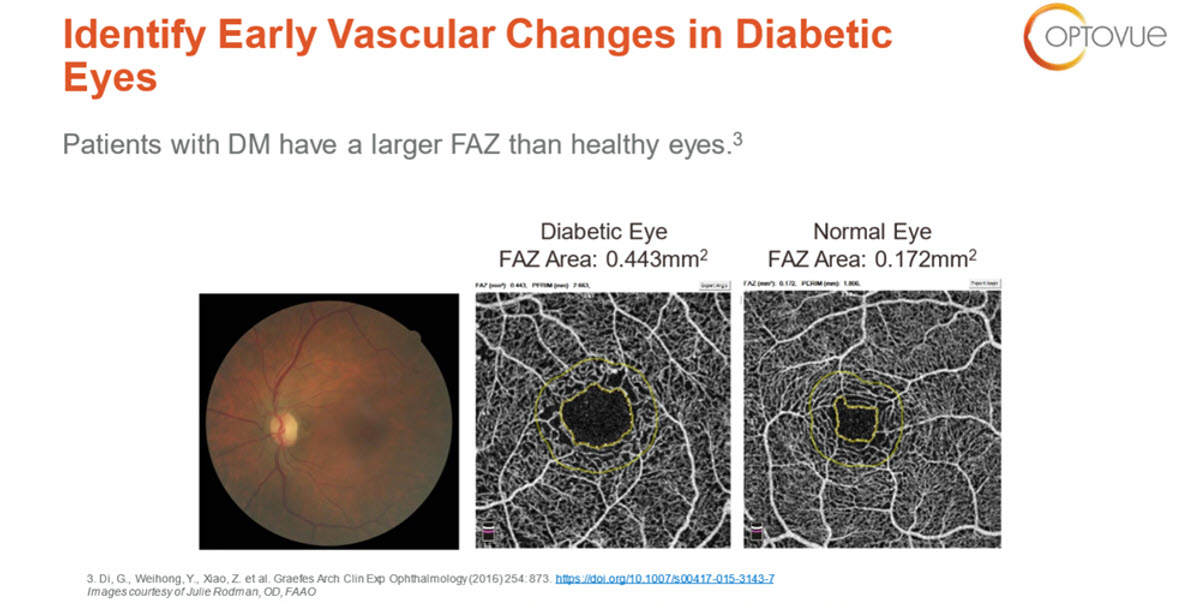
Figure 1. Left, fundus photograph of diabetic patient. Center, OCTA image of that same eye showing a large foveal avascular zone (FAZ). Right, OCTA image of normal retina with a normal, smaller FAZ.

Figure 2. OCTA image of a diabetic patient to assess vessel density over time. Looking at the traditional B-Scan OCT of 2015 and 2016 there are no visible diabetic retinopathy changes. It wasn’t until 2017 in the parafoveal area that we see exudate or hemorrhage on the B-Scan OCT. However, diabetes is a capillary disease and from 2015-2017 capillary density is decreasing significantly much earlier before visible findings on the B-Scan OCT.
Change Patient Care & Dialogue Between Providers
Utilization of this technology and information will not only change your relationship with your diabetic patients, it will change the relationship and the dialogue you have with other healthcare providers in your community, especially primary care physicians (PCP) and endocrinologists. When you are able to report OCTA results in combination with HbA1C risk assessment to the patient’s PCP, as well as the patient, you have now given the PCP and the patient information to take control of their blood sugar in a way that provides direct feedback on how effective their efforts are in reducing their risk. Practicing in this manner represents one of the main goals of healthcare reform: to engage the patient and empower them to take control of their care.
The OCTA is able to detect, measure and monitor early microvascular changes in the eye. However, it is likely that similar changes are occurring in other parts of the body including the kidney, heart, brain and all other vascular beds throughout the body. While a clinical outcome registry gives you the ability to track data on risk of developing visible diabetic retinopathy based on OCT-A results and HbA1c levels, data is also being tracked on the time period from first diagnosis of diabetes to the development of other diabetic vascular-related complications such as neuropathies, kidney failure, breakdown of skin resulting in foot ulcers and bed sores, etc. The data you provide to other physicians in your community will also help them assess the patient’s risk of developing these other complications based on your report.
Importantly, all communications you have with these other physicians are completed through Direct Messaging. This feature allows reporting directly from your EHR to the patient record in the EHR of the other physician. Armed with the data you have provided, these physicians will be excited and encouraged to refer their diabetic patients to you for their eyecare. In addition, don’t be surprised if you are invited to make a presentation on OCTA to a physician group in your community. There are numerous ways to use registry data to help discuss findings with patients and analyze prescribing, follow-up care and referral patterns. A few select examples are listed in the box below.
Examples of what registry data can be used for in combination with OCTA
- correlation between time of diagnosis of diabetes to the time when OCTA changes appear and the time period when visible retinopathy appears based on HbA1c levels
- correlation between the time of diagnosis of diabetes to the appearance of major systemic diabetic complications. Evaluation of the predictive effect of early OCT-A changes based on HbA1c levels
- how effective eye care providers are in utilizing OCTA findings in diabetic patients to engage them to lower their HbA1c to reduce the risk of developing more advance diabetic retinopathy
- how effective eye care providers are in using OCTA results to affect referral patterns of primary care physicians to refer to them for OCTA testing rather than waiting for visible retinopathy to develop
Using OCTA data, ODs will be able to educate patients about how the latest diagnostic retinal technology is helping them reduce their risk of vision-threatening complications. Combining registry data with OCTA results can be used to motivate diabetic patients to take responsibility for behavior and lifestyle changes that will promote long-term retinal health. In summary, use of this technology will enhance the quality of the care you provide to your diabetic patients, create patient loyalty and stimulate referrals from PCPs. These are advantages that pave the way to ensure the health of your practice in the future.





